Key fact

15.7 million children
in 12 countries in Africa’s Sahel region were protected through seasonal malaria chemoprevention programmes in 2017.
Featured video
The biggest challenge faced by malaria endemic countries in Africa is inadequate financing for malaria prevention and treatment services for people at risk of malaria. As a result, there are communities or populations that cannot access prevention measures or treatment when needed. In some parts of sub-Saharan Africa, mosquitoes that transmit malaria have become resistant to certain older insecticides.
Some people are more vulnerable to malaria than others. Partial immunity to malaria can be developed over years of exposure. As young children have not had the opportunity to build up this partial immunity, they are particularly at risk, and make up the majority of fatal cases of malaria in the WHO African Region.
As well as having a significant human cost, the effects of malaria extend far beyond direct measures of morbidity and mortality. Malaria can reduce school attendance, productivity at work, and there is evidence that the disease can also impair intellectual development. The economic costs are also significant. Between 1965 and 1990, countries in which a large proportion of the population lived in regions with malaria experienced an average growth in per-capita GDP of 0.4% per year, whereas average growth in other countries was 2.3% per year.
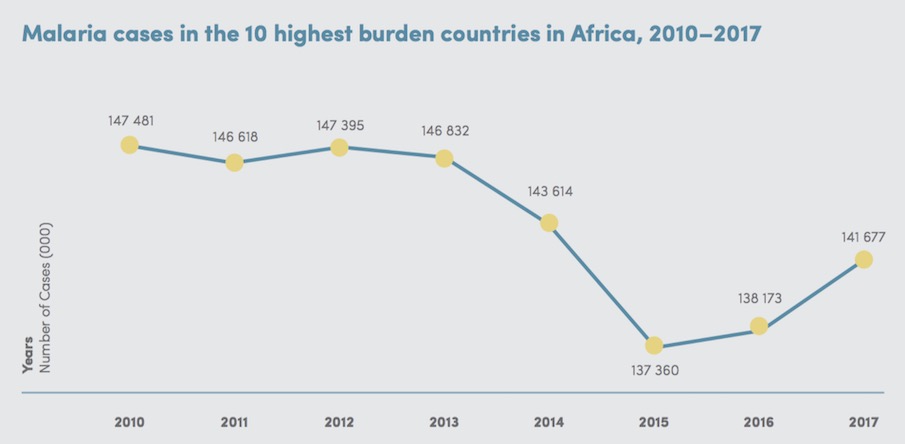
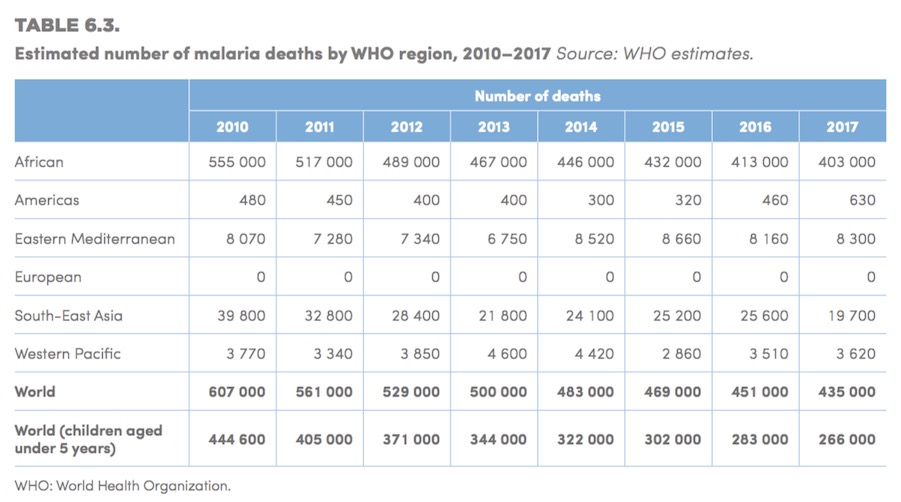
Disease burden
Malaria is widespread throughout tropical and subtropical regions of the world, and Africa carries a disproportionately high share of the global malaria burden, both in terms of total malaria cases and malaria deaths. In 2017, there were an estimated 219 million cases of malaria worldwide. Most were in the WHO African Region, with an estimated 200 million cases, or 92% of global cases. In 2017, five countries accounted for nearly half of all malaria cases worldwide. Four of these were in Africa: Nigeria (25%), the Democratic Republic of the Congo (11%), Mozambique (5%), and Uganda (4%).